Most of us take for granted being able to read a bedtime story to our children. But for Scott, who acquired aphasia after a stroke in 2008, he lives with the challenge of trying to communicate and parent his boys.
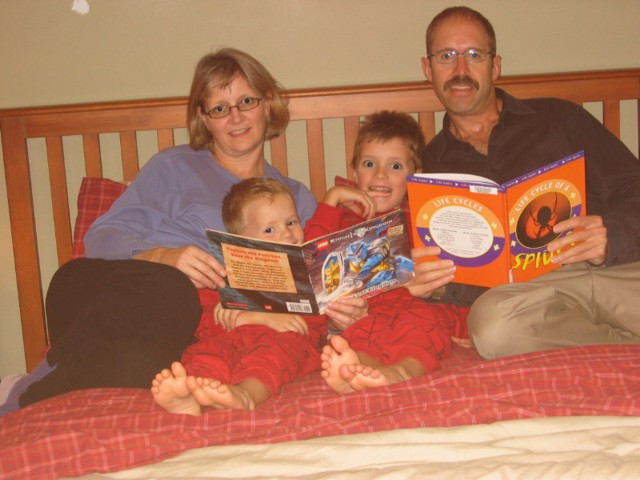
The Ardiel family piles into their big bed for a favourite nightly ritual. Jane reads a storybook aloud to her boys and husband while running her index finger along the page under the words so six-year old Ben can follow along. Sometimes Ben reads a page. Aiden, at four-years old is too young to read so he snuggles in to enjoy the tale. For dad Scott, although reading a sentence aloud is a struggle, he participates as fully as he can in this bonding family routine.
Most of us take for granted being able to read a bedtime story to our children. But for Scott, who acquired aphasia after a stroke in 2008, he lives with the challenge of trying to communicate and parent his boys. “[Aphasia] , that’s been a struggle from the beginning. [I] can’t tell [the boys how to do things], but I have to show them,” says Scott.
Even though Scott knows what he wants to say, he has difficulty expressing it. Sometimes he finds it hard to understand what others are saying and reading can be difficult. Scott and Jane found the Aphasia Institute to be a “nugget of hope” once Scott was released from rehab after his stroke. They found comfort in an environment that understood the impact aphasia had on the whole family.
Jane joined the Family Support and Education Group and found a community that empathized with her experience.
Today Scott is a member of the Toastmaster Aphasia Gavel Club and an active volunteer at the Toronto Rehabilitation Institute. Jane has made it her mission to educate every medical professional they have encountered along this journey about aphasia.
“Much of my own healing through this experience has come from the opportunity to help others. There’s a saying – we achieve happiness when we seek the happiness and wellbeing of others,” says Jane.
Jane & Scott Ardiel
Norma
